When you’re suddenly faced with a health crisis, the world can feel like it’s spinning out of control. Emergency home care is designed to be that steadying hand, providing professional support right in your loved one’s home when you need it most.
Think of it as a rapid response team for care. It can be arranged incredibly quickly—often within 24 to 48 hours—to handle a sudden illness, a complicated hospital discharge, or that difficult moment when a family carer simply can’t manage anymore.
Spotting the Signs: When Is It an Emergency?
A crisis doesn’t always announce itself. Sometimes it's a dramatic event, but just as often, it's a slow burn that suddenly hits a breaking point. Knowing what to look for is the key to acting fast and getting the right help in place.
Arranging care at home in an emergency means you can often avoid a stressful hospital admission or a frantic search for a care home bed. Instead, your loved one gets to recover in familiar, comforting surroundings. This isn't just about comfort; it's about creating a safe environment that can genuinely speed up their recovery.
The Sudden Red Flags
Some situations are unmistakably urgent. These aren't minor issues but serious events that make it unsafe for a person to be on their own, even for a day.
You might be facing a scenario like these:
- A serious fall: A fall can do more than break bones; it can shatter someone's confidence and mobility. If your parent is suddenly too unsteady to get out of a chair or walk to the bathroom safely, that’s a clear signal for help.
- An acute illness or infection: Something like a urinary tract infection (UTI) can cause sudden and severe confusion in older people. A chest infection can leave them incredibly weak and breathless. These conditions need more than just a GP visit; they require hands-on support at home.
- A tricky hospital discharge: The hospital might say your loved one is medically stable, but that doesn't always mean they're ready to cope alone. They might be discharged needing help with everything from washing and dressing to remembering their medication.
When a Slow Decline Hits a Tipping Point
Emergencies aren't always loud and sudden. More often, it's a gradual slide that finally reaches a point where the current support system—usually a family member—is completely overwhelmed.
When a family carer reaches their limit, that is the emergency. Pushing through burnout isn't just risky for the carer; it puts the person they're looking after in danger too. It’s a critical moment to bring in professional support.
Watch for these warning signs that things have become unmanageable:
- Significant changes in thinking: Is their confusion suddenly much worse? Are they forgetting important things or behaving in ways that are completely out of character? This could point to a new medical problem that needs immediate management.
- A decline in personal care: If you notice your loved one isn't bathing, is wearing the same clothes for days, or is struggling with incontinence, it's a strong indicator they can no longer manage these basic tasks alone.
- Losing weight or not drinking enough: This is a major red flag. It often means they're struggling to cook for themselves or are simply forgetting to eat and drink. This requires urgent intervention to prevent serious health complications.
Recognising these triggers is about turning panic into a plan. It allows you to take decisive action and put a professional safety net in place right when it matters most.
Your Immediate Action Plan for Arranging Care
That gut-wrenching moment you realise a loved one needs help now can send your mind racing. It feels overwhelming, but the trick is to channel that adrenaline into focused, practical steps. A clear plan is what turns panic into purpose, helping you make the right calls in those critical first few hours.
First things first: Is this a medical emergency? If there’s been a serious fall, a suspected stroke, or any other immediate danger to life, your first call is always 999. Don't hesitate. Paramedics are the experts here; they can provide life-saving treatment on the spot and decide if a trip to the hospital is necessary.
If the situation is urgent but doesn't feel like a 999 emergency, your loved one's GP should be your next port of call. They know the medical history and can often provide advice that prevents an unnecessary hospital admission, connecting you with community health services instead.
Who to Contact for Urgent Support
Once any immediate medical crisis has been managed, your focus can shift to getting care set up at home. Knowing who to call saves precious time and a whole lot of stress.
- Local Authority Social Services: Every council has an adult social services department. They're the ones who can carry out an official care needs assessment and see if your loved one is eligible for council funding. Crucially, most have an out-of-hours emergency duty team for crises that happen over the weekend or at night.
- CQC-Regulated Care Providers: If you’re planning to fund the care privately, going directly to a private home care agency is almost always the fastest way to get help. The golden rule is to only consider providers regulated by the Care Quality Commission (CQC). This is your guarantee that they meet national standards for safety and quality. Many good agencies have a rapid response team specifically for these kinds of situations.
When you're looking for help, a provider's ability to deliver compassionate urgent care services is what makes all the difference.
Preparing for That First Call
To get things moving quickly, a little preparation before you pick up the phone goes a long way. A care provider needs a clear snapshot of the situation to get the right support in place, fast. Coming to them with the key facts shows them how urgent things are and helps them spring into action.
I’ve seen it time and again: having a concise summary of your loved one’s needs, medications, and routines can literally cut the assessment and organisation time in half. It’s the single most powerful thing you can do to get a carer through the door faster.
Sometimes, the need for care comes out of the blue after an illness or accident. Other times, it's the result of a gradual decline or a family carer simply reaching a breaking point. This flowchart shows the common paths that lead to needing immediate support at home.
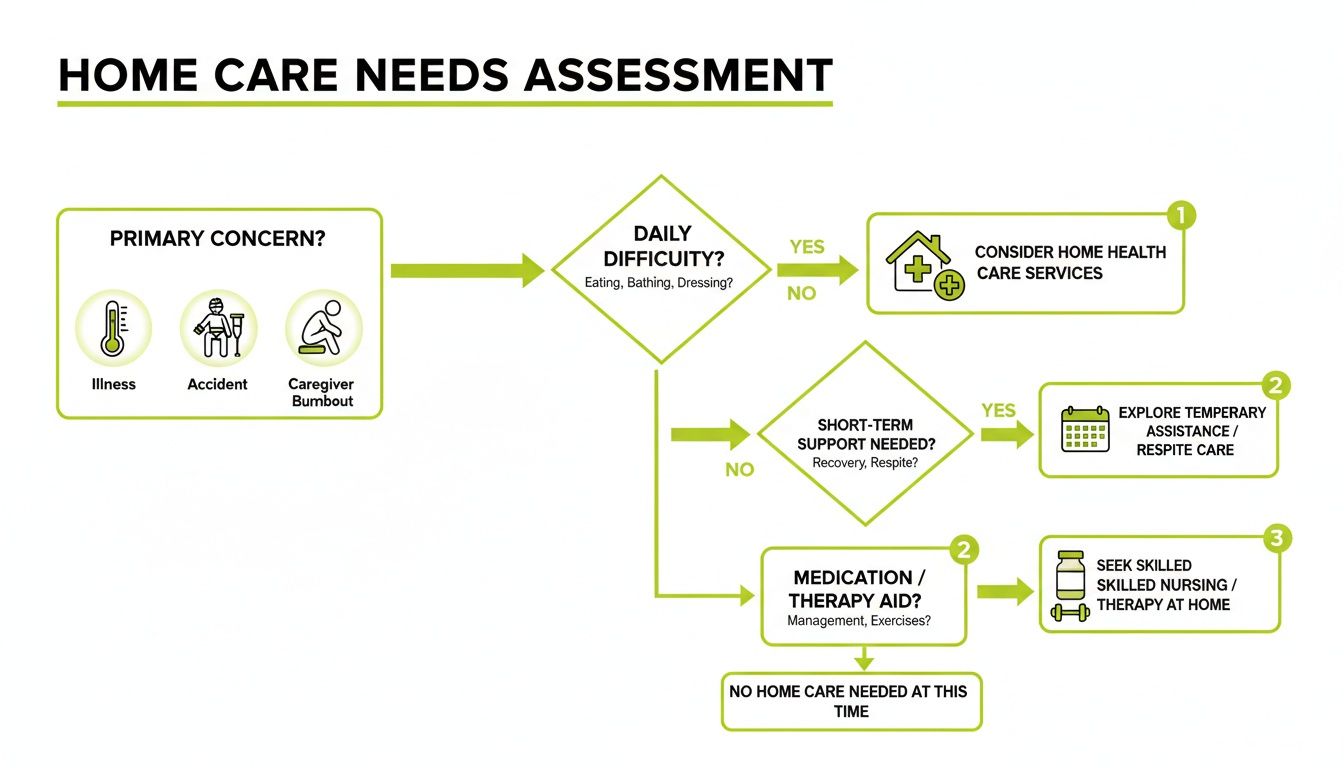
As you can see, different triggers might require slightly different first steps, but they all ultimately lead to a professional assessment to make sure the person is safe and their needs are properly met.
The importance of a well-oiled community care response was tragically highlighted during the COVID-19 pandemic. UK emergency planning was so heavily focused on hospitals that it left a massive gap. This oversight contributed to over 100,000 excess deaths at home by July 2022, with the homecare needs of nearly a million adults overlooked despite the "Stay at Home" messaging. It’s a stark reminder of why having efficient, community-based emergency care is absolutely vital.
Essential Information to Gather Before You Call
Before dialling, take five minutes to pull together these details. Just jot them down on a notepad or in a note on your phone. This simple step makes the whole process smoother and faster.
Essential Information to Gather Before You Call
| Information Category | Specific Details to Note Down |
|---|---|
| Personal Details | Full name, date of birth, address, and their NHS number if you have it. |
| Medical History | Key health conditions (e.g., dementia, heart disease, diabetes), any recent surgery, and known allergies. |
| Medication List | The names of all prescribed medications, the doses, and what times of day they need to be taken. |
| Mobility & Needs | Can they walk on their own, do they use a frame, or are they mostly bed-bound? Note any help needed with washing, dressing, etc. |
| GP & Contacts | The name and phone number for their GP surgery, plus contact details for another key family member. |
Walking into that first conversation with this information at your fingertips is a game-changer. It gives the care coordinator a clear, immediate understanding of the situation, allowing them to start matching your loved one with a suitable carer right away. It helps turn a moment of crisis into a managed, supportive plan.
From Chaos to Calm: The Rapid Assessment and Care Plan
Once you've made those first urgent phone calls, the process shifts from crisis management to practical planning. This next step is the rapid assessment, and it’s designed to happen fast. We’re not talking about weeks of waiting; a good provider will often have this sorted within hours of your call.
This isn’t just a tick-box exercise. It's a crucial conversation between the care provider, you, and most importantly, your loved one.

Usually, an experienced care manager or a senior carer will visit your loved one at home. There’s no substitute for seeing the environment firsthand. They’ll have a gentle chat to understand what your relative wants and what they’re worried about. Your input here is invaluable – you can provide the background and fill in any gaps they might not be able to express themselves.
What Does the Assessment Actually Cover?
The goal is to get a 360-degree view of the support needed right now. The care manager will ask about a few key things to make sure the plan they create is safe, effective, and truly personal.
You can expect the conversation to touch on:
- Personal Care: This is all about maintaining dignity – help with washing, dressing, using the toilet, and grooming.
- Medication: They'll need a full list of what’s being taken, when, and at what dosage. The key question is whether your loved one just needs a prompt or physical help administering it.
- Mobility and Safety: The assessor will look at how your loved one gets around. They're trained to spot trip hazards and figure out what support is needed to move safely, like getting out of bed or a favourite armchair.
- Food and Drink: They’ll ask about diet, how much they’re drinking, and whether they can make meals for themselves. Dehydration and poor nutrition can make a bad situation much worse, very quickly.
A skilled assessor does more than just ask questions. They listen. They observe. They pick up on the little things, like a specific morning routine that brings comfort or a preference for how a cup of tea is made. These details matter.
Building a Truly Personalised Care Plan
All that information is then turned into a personalised care plan. This document is the absolute foundation of good emergency home care. Think of it less as a rigid rulebook and more as a flexible guide for the carer, outlining exactly what’s needed and, just as importantly, how your loved one likes it done.
The real strength of an emergency care plan lies in its flexibility. After a crisis, someone's needs can change by the day, or even by the hour. A good plan isn't set in stone; it's a living document that adapts as your loved one starts to recover.
This ability to adapt is vital. Support might start with full assistance for all personal care, but within a few days, as strength returns, it might be scaled back to simple supervision. It’s a huge area of social care; in a single week, a staggering 499,797 people in England received CQC-regulated care at home. This figure really underscores how much we rely on these services, especially with the NHS under so much pressure. You can see the full adult social care statistics on GOV.UK.
The Core Parts of the Plan
Any solid emergency care plan will clearly define tasks and timings. This ensures that no matter which carer is visiting, the support is seamless and consistent.
Here’s what you should expect to see laid out:
- A Daily Routine: Timings for getting up, meals, medication, and settling down for the night.
- Specific Instructions: Clear details on how to help with personal care, what meals to prepare, and any mobility support needed.
- Communication Log: A vital space for carers to leave notes for each other and for you, tracking progress and highlighting any concerns.
- Emergency Contacts: Your details, the GP, and any other key healthcare contacts, all in one place.
This level of detail means every carer who walks through the door is fully briefed and ready to help, bringing a sense of order and reassurance when you need it most. It's this structured yet personal approach that shows how personalised home care supports independent living, turning a stressful situation into a managed recovery in the comfort of home.
Figuring Out the Finances and Legal Stuff
Let’s be honest, the cost of emergency home care is a huge worry for most families. When you're trying to cope with a crisis, the last thing you need is the extra stress of untangling a web of financial rules. But getting a handle on the options available in the UK can make a world of difference.
Essentially, there are three main ways to pay for care: through your local council, via the NHS, or by paying for it yourself (often called 'self-funding'). Which route is best—and fastest—in an emergency really comes down to your loved one's specific circumstances.
Getting Help From the Local Council
For many, the first port of call is the adult social services department at their local council. They’re the ones who assess what help is needed and figure out if someone qualifies for financial support. This usually involves two distinct stages.
First, they'll carry out a care needs assessment to understand exactly what support your loved one needs to stay safe at home. Then comes the financial assessment, or means test, where they look at income, savings, and other assets to calculate how much, if anything, your loved one should contribute to their care costs.
A lot of people think that owning a home automatically means you have to pay for all your care. That's not true for care at home. The value of your main property is not included in the means test for home care—it only comes into play for residential care.
The savings thresholds do change each year. As a general guide, if your loved one in England has savings and assets over £23,250, it’s likely they’ll be expected to pay for their own care.
When the NHS Covers the Cost
In some situations, the NHS might cover the full cost of care. This is called NHS Continuing Healthcare (CHC), and it's for people whose primary need is a health one, not a social one. The great thing is that it isn't means-tested, and it can be provided anywhere, including in your own home.
Qualifying for CHC involves a detailed assessment, which, admittedly, isn't always quick to arrange in a crisis. But if your loved one has complex, intense, or unpredictable medical needs—maybe after a major stroke or due to a rapidly worsening condition—it's an avenue you absolutely must explore.
The NHS has detailed guidance on the process, which starts with a simple checklist before moving to a full assessment by a team of different health professionals. It might not be an overnight fix, but for those with significant health needs, it's a critical right.
Self-Funding and Getting Your Ducks in a Row Legally
If your loved one’s assets are above the council’s limit, you'll be looking at funding their care privately. This gives you the most choice and is usually the fastest way to get help in an emergency, but it also means you need to have a firm grip on the finances and legal side of things.
This is where having the right legal paperwork in place becomes non-negotiable. If your loved one can no longer make their own financial decisions, you can't just dip into their bank account to pay the care agency, even if it’s for their own good. You need the legal authority to do so.
That's why a Lasting Power of Attorney (LPA) for financial decisions is so incredibly important. It lets a trusted person (the ‘attorney’) manage someone's finances on their behalf. Without one, you’re forced to apply to the Court of Protection to be appointed as a ‘deputy’, which is a much slower, more stressful, and more expensive route. A Durable Power of Attorney is a crucial legal document that allows someone to make critical decisions on your behalf, especially important in unexpected health emergencies.
When you're paying privately, you also need to be sure you're hiring a reputable agency. Don't just go with the first name you find. Always make sure the provider is:
- Fully Regulated: Look them up on the Care Quality Commission (CQC) website and read their latest inspection report.
- Properly Insured: They must have public and employer's liability insurance. Don't be afraid to ask for proof.
- Upfront About Costs: A trustworthy agency will give you a clear, itemised breakdown of all fees. There should be no nasty surprises.
Tackling the money and legalities can feel overwhelming, but sorting these things out early gives you a solid foundation. It means you can focus on what matters most, knowing the care is not only compassionate but also financially secure and legally sound.
Preparing the Home for a Smooth Transition
When you’re arranging emergency home care, your focus is squarely on your loved one. But taking a moment to prepare the house itself can make all the difference. A safe, practical environment helps the carer hit the ground running and ensures your family member feels comfortable and secure from day one.
Think of it in two parts: first, making the physical space safe and accessible, and second, getting all the essential information and supplies ready for the carer. Tackling this quickly means the professional can focus entirely on your loved one’s needs, not on navigating obstacles.

This isn’t just about having a quick tidy-up; it’s about creating a space that actively supports recovery and reduces risk.
Creating a Safe and Accessible Space
Safety is your first priority. A carer needs to move around freely, often while helping someone with their mobility. Try to see the home through their eyes and you'll quickly spot potential hazards.
Even small changes can have a big impact:
- Clear the Pathways: Make sure hallways, the living room, and the bedroom are free of clutter. Things like loose rugs, trailing cables, or stacks of magazines are common trip hazards that are easy to remove.
- Brighten Things Up: Good lighting is crucial, especially for any late-night trips to the bathroom. Check that all bulbs are working or consider adding a simple nightlight to guide the way.
- Make the Bathroom Safer: A non-slip mat in the shower or bath is a simple but effective safety measure. Also, make sure towels and toiletries are within easy reach to avoid any risky stretching or bending.
Making the home secure is paramount. This includes checking for less obvious dangers; for example, knowing about things like detecting gas leaks is a vital part of ensuring the environment is safe before a carer arrives.
Equipping the Carer for Success
Once the physical space is sorted, the next step is to arm the carer with practical information. They're walking into an unfamiliar home, often under pressure, so anything you can provide to give them context is a massive help.
I’ve always found that a simple folder with key information is invaluable. It saves the carer from asking endless questions and helps them see your loved one as a person, not just a patient. This one small gesture can transform the whole care experience from purely functional to truly compassionate.
Getting this right is a critical factor in successful domiciliary care. In fact, between 2024 and 2025 in England, a staggering 89.1% of people who couldn't remain in the community after a hospital stay ended up with an unplanned readmission. Effective home support, which starts with a well-prepared environment, is the key to breaking that cycle. You can discover more insights about adult social care outcomes on GOV.UK.
What to Include in a Carer Information Pack
You don't need anything fancy. Just gather the essentials in a notebook or a folder and leave it somewhere obvious, like the kitchen table. It will make the handover seamless.
Essential Information and Supplies:
- Key Contacts: A clear list of names and numbers for family members, the GP, and any other healthcare professionals.
- Medication List: The full, up-to-date list of prescriptions, including what time they need to be taken, dosage instructions, and where they are kept.
- Their Daily Rhythm: A few notes on their typical routine can work wonders. When do they usually wake up? Do they have a favourite mug for their morning tea? These little details help maintain a sense of normality.
- Likes and Dislikes: Jot down their food preferences, what they like to watch on TV, or subjects they enjoy talking about. This is gold dust for a carer trying to build rapport and provide genuine companionship.
- Household Basics: Quickly show the carer where to find essentials like cleaning supplies, fresh towels and bedding, the fuse box, and the main water stopcock.
Taking these steps shows you're working as a team and sets a positive tone from the very beginning. It helps the carer feel supported and ready, allowing them to provide the best possible emergency home care right away.
From Crisis to Calm: Transitioning to Long-Term Support
An emergency home care package is designed to be a lifeline, getting you and your family through a crisis. But it's usually just the beginning. Once the immediate pressure is off and things have settled, it's time to think about what comes next. The focus needs to shift from urgent, reactive support to a sustainable, long-term plan that helps your loved one truly thrive.
The plan you put together in a hurry was all about speed and safety. Now, you have the breathing room to refine it. Sit down with the care provider and have an honest chat. What's working brilliantly? What isn't? Perhaps your loved one has regained some independence and doesn't need as much help with certain tasks. This is a collaborative process, all about fine-tuning the support to match their recovery and changing needs.
Taking Stock of Ongoing Care Needs
As the dust settles, you can start planning more strategically. The goal is to build a proactive support system that genuinely enhances their quality of life, not just gets them through the day. Think about what a 'normal' week looks like now and identify where the support gaps still are.
This might lead you to explore different, more permanent care arrangements.
- Regular Domiciliary Care: This could be anything from a daily visit for help with washing and dressing to a few calls a week for a bit of shopping and companionship.
- Respite Care: Absolutely crucial for family caregivers. Respite gives you scheduled, reliable breaks to rest and recharge, confident that your loved one is being well looked after.
- Specialised Support: If you're dealing with a progressive condition like dementia or complex medical needs, now is the time to find a provider with the right specialist skills and experience.
From my experience, the best long-term care plans are built on a foundation of open, honest communication. Regular catch-ups with the care team and your loved one are non-negotiable. It’s the only way to ensure the support stays relevant and genuinely helps them maintain their independence, rather than creating dependence.
Building a Support Strategy that Lasts
Creating a sustainable care strategy is less about ticking boxes and more about establishing a stable, comforting routine. You want to move towards having a consistent team of carers who get to know your loved one’s quirks, preferences, and personality. When that happens, the relationship transforms from a simple service into a real, trusted partnership. This stability is often the key to helping someone feel truly safe and happy in their own home.
The journey from a crisis to a calm, manageable routine doesn't happen overnight. Our guide to arranging home care services in 5 simple steps breaks down how to create a more structured plan for the long haul. By carefully managing this transition, you can make sure the initial emergency support evolves into a solid foundation for your loved one's long-term health and wellbeing.
Common Questions About Emergency Home Care
When you’re suddenly faced with arranging urgent care, your head is likely swimming with questions. It’s completely normal. Let’s walk through some of the most common things families ask, so you can feel a bit more prepared and in control during a stressful time.
How Quickly Can Emergency Home Care Be Organised?
This is usually the first thing on everyone’s mind. In a true crisis, speed is everything. The good news is that many reputable UK providers, especially those with dedicated rapid response services, can often get an assessment done and have a carer in place within 24 to 48 hours.
Honestly, how quickly it happens often comes down to the information you can give them. The more prepared you are on that first phone call—with a clear picture of your loved one's needs, their medication list, and daily routine—the faster they can move. It helps the provider pinpoint the right professional for the job without any delay.
What’s the Difference Between Emergency Care and Respite Care?
It’s easy to get these two mixed up, but they serve very different purposes. Knowing which one you need helps you ask for the right kind of support from the get-go.
Emergency home care is purely reactive. It’s for when a crisis hits out of the blue – a sudden fall, an unexpected illness, or a loved one being discharged from hospital much sooner than you anticipated. It’s all about getting immediate, safe support in place.
On the other hand, respite care is usually planned in advance. It’s designed to give a regular family caregiver a scheduled break. This is vital for preventing burnout and ensuring you can recharge, knowing your loved one is being looked after by a professional.
Think of it this way: emergency care is the social care equivalent of an ambulance, arriving when a crisis hits. Respite care is more like a planned check-up that keeps the whole family healthy and supported for the long haul.
How Do I Know if a Home Care Provider Is Trustworthy?
Letting someone into your family’s home is a massive leap of faith, especially when you’re feeling vulnerable. Thankfully, there are clear signs of a quality provider in the UK that can give you real peace of mind.
The single most important thing to check is their regulatory status. Make sure any provider you consider is registered with and rated by the Care Quality Commission (CQC). You can look up their latest inspection reports right on the CQC website – it’s all public information.
Beyond that, a little digging goes a long way:
- Look for recent, genuine reviews from other families.
- Ask them directly about their staff vetting process, including DBS checks.
- Find out what kind of training their carers receive, particularly for specific conditions like dementia or post-stroke care.
A good, trustworthy agency will be completely transparent and happy to answer every single one of your questions. If they’re evasive, that’s a red flag.
Can We Choose the Carer Who Comes into Our Home?
In a true emergency, the provider’s top priority is getting a skilled and appropriate carer through the door as fast as possible. This means you likely won’t be able to hand-pick a specific person for those first few critical visits.
However, a great agency won’t just send anyone. They’ll work hard to make a thoughtful match based on the skills needed and, where possible, on personality. Once the immediate crisis settles down and the arrangement becomes more regular, you’ll have much more say. The goal is always to build a consistent, familiar team that your loved one can feel comfortable with.
At Cream Home Care, we know that a crisis doesn’t stick to a 9-to-5 schedule. Our compassionate, professional team is always ready to provide rapid and reliable emergency home care to support your family when you need it most. To find out more or arrange urgent support, please visit us at https://creamhomecare.co.uk.






